Women of color share struggles, experiences of healthcare profession
March 23, 2021
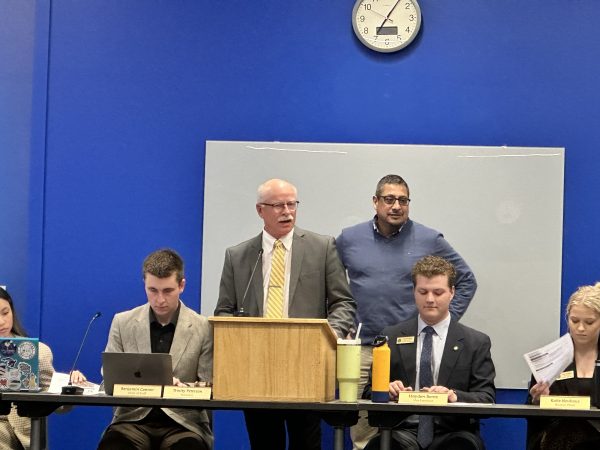
In honor of National Women’s History Month, South Dakota State University’s Multicultural Center recently hosted a panel of women of color to share the challenges and experiences of Black, Indigenous, People of Color (BIPOC) female health professionals.
The Health Professionals of Color Panel March 18 featured four women in various health care positions: Ayoko Quevison, a doctorate student for the nursing anesthesia program at Mount Marty University; Beverly Warne, a mentor for SDSU’s nursing program at the Native American Nursing Education Center in Rapid City; Paula Bennett, MD, a traveling physician and holistic provider and Tiffany Niemann, the laboratory support specialist for the Medical Laboratory Sciences (MLS) program at SDSU.
“I think it’s good for getting some people in front of students who can give them different perspectives,” Alex Wood, retention adviser for African American programs, said. He gave credit for the idea to Dakota Barnes, Black Student Alliance treasurer, who initially suggested the idea for the panel to him.
The event kicked off by asking each panelist how they became involved in a healthcare profession.
Bennett said she had wanted to be a physician since her mother passed away from health complications when she was a young girl in Jamaica.
Since then, she has grown to love the science of medicine and works with people to help their bodies heal themselves through treatment and support.
“As a physician, I am the teacher who lovingly reminds my patients of this forgotten talent of theirs, as I assist and support their bodies, minds, spirit and hearts through these healing processes,” she said.
Quevison said she grew up around many nurses in her home country of Togo in West Africa, and she received her nursing license there, working as a home health aide for elderly patients.
She later became interested in the anesthesia field, and after working at a few different hospitals, she was eventually accepted into the program at Mount Marty, though according to her, there are historically very few nurse anesthetists of color.
“This is a profession that has been around for 150 years, yet only 11% of the CRNAs (Certified Registered Nurse Anesthetists) that are practicing are minorities, and of that 11%, only 2% are African American,” Quevison said.
She also added that in her cohort of 32 students, only three are minorities: Quevison, her roommate and one Hispanic student.
The other panelists also shared examples of challenges they have seen or experienced as BIPOC women in healthcare.
Niemann said, as a Hispanic woman, she often faced stereotypes of being unsuccessful or “not amounting to much” because of her ethnicity.
“Getting into the healthcare field, I personally saw it as a personal challenge to myself to not necessarily prove everybody wrong, but to prove to myself that I could beat that stereotype,” she said.
She also added after the panel that one of the biggest challenges BIPOC women face in healthcare other than racism is a lack of mental health resources.
“I don’t think enough attention is brought to the burnout, the stereotyping and the stresses that the field can bring for women of color,” Niemann said.
Bennett and Warne also mentioned disparities in healthcare between BIPOC and white patients, especially in the last year during the COVID-19 pandemic. Bennett attributed a few reasons as to why many minorities fall victim to COVID-19 and other health issues more frequently than white patients.
“The first piece of it is this: insurance,” she said. “Do we have the insurance to meet our needs? Either it’s substandard insurance or subpar insurance, or you have no insurance at all.”
She also pointed out that many BIPOC people cannot access medications for diabetes, high blood pressure or high cholesterol, and these types of medications are often used to help combat COVID-19 cases. Those who are already on these drugs—most often white patients— have a lower chance of experiencing severe COVID-19 symptoms than those who are not taking these medications.
Warne, who grew up on the Pine Ridge Indian Reservation and is a member of the Oglala Sioux Tribe, said historically, Indigenous peoples have always struggled to get proper healthcare, and the Indian Health Service (IHS), a program meant to provide medical services to tribal communities, has never been properly funded.
“IHS has been poorly funded all these years, and that is a huge part of the problem,” she said. “We don’t have enough funding for the prevention programs that we know are so important to teach the children proper behaviors and healthcare behaviors early on.”
Some of the panelists offered some advice on how to stay hopeful in the face of issues like a lack of acknowledgment of racism. Quevison stressed the importance of “knowing you are good enough” despite what others might think or say.
“When you’re in that situation, the best thing to do is educate them and don’t get upset,” she said. “Let your approach show them that the way they think of you is false.”
The panelists also shared how students and future healthcare professionals can help to reduce these disparities in patient care.
“Whoever you take care of, whoever you are in contact with … be a role model for them, of behavior, and being open to all cultures, that is very powerful, especially from a person who is not of color,” Warne said.
Niemann added a piece of advice her father told her as a child that she thinks applies not only to everyday life, but to healthcare, as well.
“He said, ‘you just remember that you are no better and you are no worse than the person who is sitting right next to you, so treat them as such,’” she said.
After the panel, some panelists also shared how predominantly white colleges, like SDSU, can better support their BIPOC healthcare students. Niemann mentioned how education is one of the most important aspects of both improving BIPOC student retention and improving BIPOC patient care.
“I think if healthcare problems can find a way to incorporate scenarios or case studies about BIPOC individuals and how to ethically care for them without racial bias is huge,” she said
Quevison said hiring more diverse faculty in healthcare programs and doing more to recognize the financial differences between white students and students of color could also help.
“Students of color may not have familial financial support and may graduate with a higher amount of debt than their white peers,” she said. “PWI (primarily white institutions) should recognize this by ensuring that these students are provided with sufficient grants and loans.”
Livia McFadden, a nursing major who attended the event, said she learned how to respond to discrimination and racism in the workplace. She also said she thinks the event helped to show how empowered women can be.
“I think a lot of the time we’re fighting so hard to just be recognized as powerful and important to society,” she said. “And we get told what to do with our bodies and our minds and everything, and it’s nice to be reminded that we don’t have to listen, and we can do anything we want, even when society tells us we can’t.”